TUBERCULOMA VERSUS NEUROCYSTICERCOSIS-BRAIN
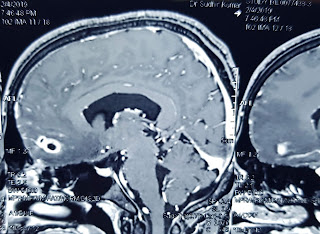
TUBERCULOMA VERSUS NEUROCYSTICERCOSIS BRAIN Solitary granulomatous lesions are common causes of seizures and headache in India and elsewhere. The two most common causes are: 1. Tuberculoma (caused by Mycobacterium tuberculosis), 2. Neurocysticercosis-NCC (caused by tapeworm, Taenia solium). Treatment involves 1. Use of antiepileptic drugs for seizure control, 2. Specific anti-infective treatment for for TB or NCC. Anti-tuberculous treatment is long and may be needed for 18 months or longer. For tapeworm infection (NCC), 1-2 week treatment may be enough. Appropriate treatment depends on confirmation of diagnosis. The gold standard for confirming the diagnosis is biopsy of the lesion, which requires surgery in brain. Therefore, practically diagnosis depends on MRI and CT scan features. MRI features favoring a diagnosis of tuberculoma are: 1. Size> 2 cm, 2. Severe perilesional edema, 3. Conglomerate lesions. Presence of focal neurological deficits also favor a diagnosis of tu